So, here’s the thing. A few years into running my blog and starting up my freelance work, I realised that I’d never actually sat down to write my own chronic illness story. I think there were a few reasons why I was hesitant, and why I’m still somewhat hesitant now. Being a chronically ill or disabled person online comes with a torrent of unsolicited advice, incorrect assumptions, and often hostility… and most of the time, it’s coming from complete strangers. Lucky us, hey?
I also wondered if there was any real ‘point’ to telling my story, or whether I needed to share so much of myself in order to be an advocate. After all, no two people experience chronic illness the same, our lived experiences can be so different from each other, and I firmly believe that everybody has their own unique path to follow. What could anybody else possibly gain from reading my story?
However, I recently had cause to reflect back on my own early years with chronic illness. It would be difficult to forget the confusion, fear, and grief I experienced during those days, never mind how it felt to discover the profound lack of support and information available for patients at that time. One of the things that helped me make sense of it all was finding the chronic illness community and engaging with other people’s blogs and social media posts. Even if our circumstances differed (illness severity, age, geographical location, and so on) reading about others’ experiences played an important role in helping me tentatively figure out the next steps for myself.
So, whilst it’s incredibly important to highlight that my story is my own and not in any way representative of every person with ME/CFS, I’m putting it out there in case it’s in any way helpful. Here’s how it all went down…

Illness Onset
As a child, I was selected for elite training in classical ballet with a leading British company. From the age of ten onwards I began vocational training, fitting long hours in the studio, travel, and performances around my schoolwork. It’s an incredibly tough industry, and as any other dancer will know, you’re taught to push yourself far beyond what you think are your physical capabilities, ignoring any pain in the process if you’re to have any hope whatsoever of succeeding. It’s an approach that naturally becomes ingrained in everything you do, and soon you’ll see how that played out for me.
I experienced some rather nasty injuries throughout my training, and around the age of fifteen, as I was making important decisions about my future, two things happened in rather quick succession. Firstly, I experienced a life-threatening anaphylactic shock: a severe allergic reaction to what we later found out was peanuts, after indifferently eating a handful of the pesky things for the first time at a house party. It was a frightening and a horrific experience that I’m in no hurry to repeat, but fortunately I bounced back rather quickly… only to subsequently develop glandular fever.
Now, the key to managing glandular fever is to really take care of yourself, rest, and most importantly, avoid mentally or physically overexerting yourself. So straight off, you can see how this might have been something of a problem for me…. and that’s before you take into account that at that time, I had *no idea whatsoever* that I even had glandular fever. Although I went to the doctor multiple times during this period, with what I thought back then was just a persistent seasonal illness, it wasn’t until years later (following a retrospective blood test) that I found out this was going on back then.
So, whilst my poor immune system was going through a bit of a crisis, there I was: bulldozing my way through life. Although I was no longer training intensively in ballet, I was pushing through in the only way I knew how: squashing down the increasing feelings of poorliness, seeing them as a personal failure on my part rather than listening to those very early warning signals my body was sending me.

Although there’s been no definitive cause or trigger for ME/CFS identified yet, knowing what I know now, I have reason to believe my immune system was severely compromised following these two events (the anaphylactic shock and the glandular fever), and then further aggravated by my busy and active lifestyle when I should have been resting and recuperating.
Searching For Answers
It was shortly after this time, during my upper years at secondary school, that I first started to notice the mild but unrelenting symptoms. There were constant headaches and sore throats, feeling as though my head was full of cotton wool, and above all else, my strong and supple body and limbs feeling weak with fatigue. The same burn I’d feel in my muscles after a 10-hour day of ballet training, I felt from walking up a flight of stairs at school. Although persistent and at this point unexplained, these symptoms were still very much at the mild end of the spectrum. They rarely prevented me from carrying on with day-to-day activities, but simply made me feel hideous during them instead.
Increasingly fearful, I continued to see my childhood GP and tried to verbalise what I was experiencing. hoping for a course of medication that would set me back on track. However, although the doctor acknowledged the fatigue I was experiencing, as well as my energetic lifestyle and background, it was their belief that to combat fatigue, I simply needed to increase my stamina and physical fitness levels. They suggested taking a daily hour-long walk after school… despite the fact I’d been undergoing intensive physical dance training for most of my life. And me being the compliant teenager I was, I very much took it to heart.
I describe my experiences of being inappropriately prescribed exercise therapy in this piece for HuffPost, but in short, I experienced some quite frightening results. Rather than seeing my capabilities increase, as you would expect as my physical strength improved, the opposite occurred. Each time I walked or ran a considerable distance, I found that I could do a little less the next time. I could no longer get through intense but achievable ballet exercises I could once do in my sleep. The harder I was trying to increase my activity levels, the more irreversible harm it was doing to my body. And yet I still didn’t see it as the red flag that it was. It never occured to me that perhaps I should stop – if anything, it made me feel as though I just needed to try harder.
The Relapse
As my symptoms were still relatively mild, I continued bulldozing through life. I completed my school exams and most of my first year of university, taking on dozens of extracurricular things that I genuinely loved and trying my best to keep happy. It was only during my final term of the academic year that things took a turn. And because life is never straightforward, I was working abroad as a sports coach in Greece when I finally broke.

At that point, it was impossible to ignore that I was experiencing something life-altering. I just about managed to get home before things really spiralled, but from this point onwards, life was a completely different story. Every persistent symptom intensified, and they were joined by some delightful new friends too: chronic pain, long-term insomnia, extreme sensitivity to noise and light, allergies and chemical sensitivities, dizziness and orthostatic intolerance, and this constant feeling of just… unwellness. Like constantly being gripped by the worst kind of flu, the kind where any small exertion makes you feel more hideous. Sometimes I’d wake up from broken sleep and feel like I couldn’t catch my breath, or like there were bricks piled on top of my chest.
I’m just thankful that this difficult period took place over a long university summer. I had three months to rest (spending only a few hours out of bed per day) and try to process what was happening. It was incredibly fortunate that my parents had some awareness of ME/CFS and recognised the signs and symptoms. After years of trying and failing to access help, it took my mum physically coming into a GP appointment with me and standing her ground before I was finally referred to my local specialist service.
Finding A Diagnosis
ME/CFS is incredibly difficult to diagnose, and it often takes patients years to find the answers they’re looking for. It’s a diagnosis of exclusion, meaning in my case, multiple blood tests were carried out to rule out other chronic conditions, a thorough assessment with a clinical psychologist was undergone, and importantly, symptoms needed to have been documented for over four months before a diagnosis could even be considered – luckily by this point, I had almost four years under my belt. There’s a lot of debate in the chronic illness community over differences in terminology and diagnosis: the general consensus is that ‘chronic fatigue’ is a symptom rather than a diagnosis, with ‘chronic fatigue syndrome’ a differential, shorter-term, and often less severe diagnosis to that of ‘Myalgic Encephalomyelitis’. However, I got the best of both worlds: in October 2014, at the age of 19, I was diagnosed with ME/CFS.

Getting a diagnosis is important, but when you’re experiencing a notoriously under-researched condition, your next steps are very much limited. With no treatment or cure for the condition, the vast majority of patients are sent away to just get on with it, and hopefully learn to manage their symptoms as best as possible. After I received some well-intentioned but mostly useless booklets on pacing, activity management, and diet and nutrition, plus a one-to-one session on study skills with ME/CFS from my local service, off I went, back home to my darkened room. I had my diagnosis, but as for a prognosis? To this day, there’s no real or quantifiable method of predicting how long somebody’s symptoms will persist, or if or when they could recover or experience relief. And to me, that uncertainty remains one of the most difficult elements of living with ME/CFS.
It feels important for me to acknowledge at this point that although my physical health was a mess, my cognitive symptoms were nowhere near as severe or disabling as many other people experience. Although I had (and still have) some issues with brain fog and short-term memory, I have never experienced the profound confusion, inability to focus, blackouts, and memory loss that many people with ME/CFS live with. I could still think clearly, comprehend stimuli, and even at my worst, I could concentrate on books and TV in short bursts of around 10-20 minutes, provided I had rest afterwards. Because of this, I knew I wanted to return to university for my second year and continue my studies.
Chronic Illness and Student Life
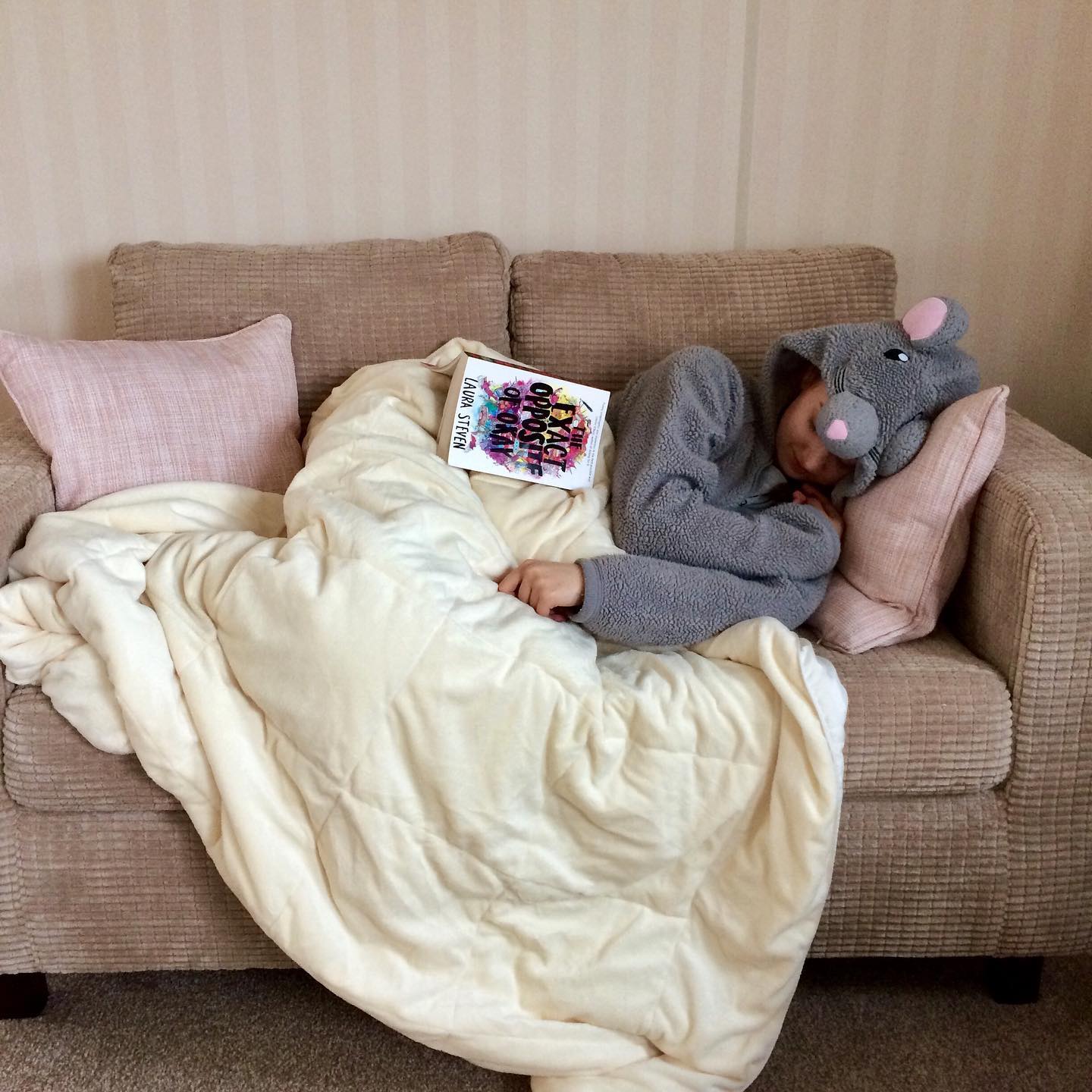
You can read plenty more about my experiences of university and chronic illness in my debut non-fiction book, University And Chronic Illness: A Survival Guide… but looking back now, it seems almost unbelievable that I managed to study full-time, live with friends and even have something of a social life during the final two years of my undergraduate degree. I still spent most of my time in bed, working from my laptop, and because I didn’t feel well enough to get to contact hours, I taught the majority of the course content to myself. A typical day would see me wake up, eat breakfast, work for a couple of hours from bed, have lunch, rest for another four hours, read notes, then eat my evening meal and spend some time in the house with friends, before going back to bed for a sleepless night and doing it all over again. When I was at my worst, I wouldn’t leave the house for weeks at a time, with any small trip out and about taking at least 48 hours of post-exertional malaise to recover from. And that was in spite of planning, pacing, and using a transit wheelchair to make these things possible.
Although I was grateful to be clinging onto student life, it was an incredibly bleak time. Keeping my spirits up wasn’t easy, but there were good people around me. I had family who helped where they could, and friends who went out of their way to keep me smiling. Even though I spent most of the time squashing down and making light of how I felt around other people, being in that kind of environment helped me cling on to some sense of normality, whilst I adjusted to my new normal.

Engaging with the online chronic illness community at this point in time played a pivotal role in this too. Through social media, I made some firm friends and found people to look up to. I also began documenting my own experiences – I had always been a writer and so it felt like a natural transition. At the time, I had no idea just how much starting up my blog and social media platforms would go on to change my life.
As much as I wish I could tell you I made complete peace with my situation, found a miracle drug and experienced a miraculous recovery, the reality is much less exciting. I am still very unwell with my condition, and it still dictates every moment of my day. However, through connecting with others and working with an occupational therapist, I began to learn how to better manage the condition and make things work for me. It was towards the end of 2016 that I first began to notice some subtle improvements, mostly in terms of pain levels and feeling a bit less… breakable, I suppose, in everyday life. Since then there have been ups and downs, fluctuations in my condition and my capabilities, but at the time of writing, I am at the strongest I’ve been since that initial relapse in 2014.

Learning To Live Again
Over these last few years where my condition has been more manageable, I’ve graduated, completed a postgraduate diploma, and now work part-time from home. I started off in the charity sector, before taking a leap of faith and becoming a chronically ill freelancer. Having the kind of career I have today would have been completely unthinkable at the beginning of this journey. I can live independently in my little flat, and I feel as though I have a decent level of autonomy and control in the choices I make as an adult. With mobility aids and adjustments, I can leave my house somewhat regularly and enjoy a social life, and recover from this much more quickly than I used to. Generally, I feel a bit more resilient to the challenges of life with a fluctuating health condition.
One of the reasons I wanted to share this post is because I don’t think people hear stories like mine as often as they should. Usually, the stories we’re told about long-term illness follow one of two narratives. Firstly, there’s the people who were once very unwell, and thanks to their sheer determination or possibly a miracle product they’re trying to sell, have made an incredible full recovery. Alternatively, there are the ones who don’t get better or regress… the ones that society tells us we should pity and feel sorry for, seeing them as a reminder that our lives could always be worse.
You don’t see many posts from us in-betweeners, the ones who’ve experienced bad health to better health without falling at either end of the spectrum. My illness hasn’t magically gone away, and I still suffer greatly because of ME/CFS. My condition still dictates every decision I make, and ableism in the world around us makes life much harder than it should be. However, my quality of life today is so much better than it was a few years ago, and it’s my belief that the chronic illness community doesn’t hear these kinds of stories enough. I hope anybody reading this knows that even if a full recovery seems unrealistic, it’s not unthinkable that things *can* improve and you can start to feel more like ‘yourself’ again.

My condition and illness severity have been relatively stable for the last couple of years, with only minor seasonal and situational fluctuations. And as of now, I don’t know what the future holds. My health could improve a notch again in the future, or it could just as easily decline back to how it was at the beginning… perhaps even worse. All I know is that although things are still difficult, and sometimes it feels as though nobody in the world could possibly understand what it’s like, the way I live now is all I’d hoped for a few years ago. The bad days I experience now were once my good days.
As humans, I think we’re conditioned to always want more than we have, or think ‘if only I could manage this little bit more, I’d be happy’. I’m definitely guilty of that. But my goodness, I’m incredibly grateful for what I have now, and I will never take it for granted. I’m doing what I can with what I have, and I’m getting better at recognising that that’s enough. And no matter what your own circumstances are or what they allow, I hope you know that your enough is absolutely enough too.
You can find out more about ME/CFS in the UK by visiting Action For ME. Please note that I am not a medical professional and cannot offer advice on your symptoms or diagnosis: if you have any concerns about your health, please book an appointment with your GP. As mentioned previously, please do *not* send unsolicited advice, no matter how good your intentions may be. Thank you.
You can also find my other chronic illness posts here, shop my books and eBooks, and don’t forget to subscribe to see my future updates too. Thanks for reading, and I hope today’s a good’un!
Related Posts:




15 Responses
Thanks for sharing your story and all the passion you bring to raising awareness!
Thank you so much, Daniel!
Thank you for sharing your story Pippa. You’re such an amazing writer and i totally echo daniEl’s comment on your passion for raising awareness. Thank you.
Thank you so much, Sophie!
I know I definitely needed to read this, and I know a few others who need to read this too. Thank you for sharing your story, it fills me with hope!
Thank you so much Niamh, I really do appreciate it!
Thank you for sharing this. I, To, have ME/CFS, which got much worse recently. I’ve since been improving gradually, but sometimes I worry that I’ll never get to live independently. this post gives me some hope that it’s possible..
Thank you so much for reading lovely, and I’m truly glad to hear that. Thinking of you x
Hey Pippa,
I came across your article on a theatre website and found my way to your article here. Firstly, well done you for making things work despite the illness and secondly, for raising awareness. I’ve been recovering from ME/CFS for 8-9 years and have a very similar story to you (pushing too much, glandular fever, etc). I too consider myself one of the lucky ones, as I seem to be able to live a ‘normal’ life, albeit with pain and symptoms that vary in intensity from day to day (the invisible fight…). I too had a frustrating journey through the healthcare system and was basically left to my own devices after the specialists offered me graded exercise therapy, occupational therapy and anti-depressants. Basically, they did their best but the rest was up to me…
Through the research I’ve done, it is possible that the Autonomic Nervous System (think fight/flight/rest/digest/etc) is central to the dysfunction. I’ve had good results from following a recovery program that bases its strategies around the idea that the ANS is reacting to triggers in inappropriate ways.
Here’s a few things that have helped me (in no particular order):
– Daily meditation
– CBT forms to address stressful thoughts/events
– A solid sleep routine
– Healthy and varied diet (lots of vegetables, cutting out processed food, caffeine and alcohol)
– Helping the gut do its job (high fibre diet, for example)
– Getting exercise, but not pushing beyond one’s energy ‘envelope’
– Having understanding family/friends/partners
Unfortunately for me, I also have a low white blood cell count (maybe from the virus?!) so have to take precautions against infections.
Anyway! I hope this post is of use to someone.
Best of luck Pippa!
Dan
Thank you so much for reading and for sharing your experiences Dan! I really appreciate the good vibes and mindful way you’ve shared your experiences. Hope today is as kind as possible to you!
Thank you so much for sharing your story Pippa. My 15year old daughter is into her second year of living with MCAS (Mast Cell Activation Syndrome) and it is really helpful for us all to read stories of how others have learnt / are learning to manage and live with a chronic illness. We have learned a lot in two years but still feel there is so much more for us to learn and your posts and books are a great resource. Thank you.
Thank you so much for your kind words Lesley, sending only good wishes to you and your daughter xx
Pippa I just wanted to give my heartfelt thanks for sharing your story and for your whole website. It makes life a little more manageable for people like me who have ME. Sending warm wishes
I’m so glad to hear it! Thank you so much for your lovely words, I really do appreciate it. Hope today’s as kind as possible to you xx
Pippa thank you for sharing your story with us and being vulnerable. I tried that I got insensitive comments back. After that I stopped sharing.
My story started after having 2 MMR shots in a month, Tdap and TB shots to work in a hospital. I was 50 at the time. 1st shot, 24 hours later developed migraines every morning. Still to this day, 13 years ago. 2 weeks later high blood pressure and chronic fatigue. I kept on working through taking excedrin, coffee, cokes to keep me functioning. I did this for 6 years. I couldn’t do it anymore.
I try to walk a mile every day. I don’t always get to due weather or just fatigued. I’ve recently been seeing a naturalopathic doctor. He’s diagnosed me with heart issues, and a peptic ulcer among other things.
I’m a fighter, researcher and pray alot. My word this year is “HOPE” and RESET this body Lord!! I’m still waiting!!